In chemotherapy-naive patients with metastatic melanoma, progression-free survival (PFS) was significantly longer with nab-paclitaxel, compared with dacarbazine, according to results from a phase III trial.
Median PFS for the nab-paclitaxel arm vs. the dacarbazine arm was 4.8 vs. 2.5 months, respectively (hazard ratio, 0.792; 95% confidence interval, 0.631-0.992; P = .044). Overall survival was similar in the two arms: 12.6 months for nab-paclitaxel vs. 10.5 months for dacarbazine (P = .27). The nab-paclitaxel group had an increased, but not significant, overall response rate (15% vs. 11%) and a significantly improved disease control rate (P = .004). The disease control rate reflects the number of complete responses plus partial responses plus stable disease for 16 or more weeks.
Nab-paclitaxel benefited patients regardless of BRAF mutation status, noted Dr. Evan Hersh, professor of medicine at the University of Arizona, Tucson, and colleagues.
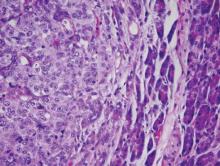
“Additionally, in a post hoc analysis of this trial, nab-paclitaxel was shown to benefit a subgroup of patients with low or absent TILs [tumor-infiltrating lymphocytes], a poor prognostic factor in melanoma,” they wrote (Ann Oncol 2015 Sep 26. doi: 10.1093/annonc/mdv324).
The most common treatment-related adverse events of grade 3 or greater were neuropathy (25% vs. 0%), neutropenia (20% vs. 10%), and leukopenia (12% vs. 7%) for the nab-paclitaxel and dacarbazine arms, respectively. The median onset of grade 3 or greater peripheral neuropathy was 101 days after treatment began.
Between April 2009 and June 2011, the multicenter, phase III, randomized, controlled trial enrolled 529 adults with stage IV malignant melanoma who had no prior cytotoxic therapy.
A majority of participants from both treatment arms underwent post-study therapy, including newer agents such as BRAF inhibitors and ipilimumab. This may account for the diminished treatment affect of nab-paclitaxel on overall survival, compared with the more significant benefit in PFS observed early in the study.
A biomarker analysis found no correlation between tumor expression of the albumin-binding protein SPARC and PFS with nab-paclitaxel treatment. SPARC was hypothesized to enrich nab-paclitaxel in the tumor microenvironment thereby increasing its efficacy.